Tranylcypromine (Monograph)
Brand name: Parnate
Drug class: Monoamine Oxidase Inhibitors
- MAO Inhibitors
- MAOIs
VA class: CN602
Chemical name: (±)-trans-2-Phenylcyclopropylamine sulfate
Molecular formula: (C9H11N)2•H2SO4
CAS number: 13492-01-8
Warning
- Suicidality
-
Antidepressants may increase risk of suicidal thinking and behavior (suicidality) in children, adolescents, and young adults (18–24 years of age) with major depressive disorder and other psychiatric disorders; balance this risk with clinical need. Tranylcypromine is not approved for use in pediatric patients. (See Pediatric Use under Cautions.)
-
In pooled data analyses, risk of suicidality was not increased in adults >24 years of age and apparently was reduced in adults ≥65 years of age with antidepressant therapy compared with placebo.
-
Depression and certain other psychiatric disorders are themselves associated with an increased risk of suicide.
-
Appropriately monitor and closely observe all patients who are started on tranylcypromine therapy for clinical worsening, suicidality, or unusual changes in behavior; involve family members and/or caregivers in this process. (See Worsening of Depression and Suicidality Risk and Pediatric Use under Cautions.)
Introduction
Non-hydrazine derivative, nonselective monoamine oxidase (MAO) inhibitor antidepressant; structurally similar to amphetamine.
Uses for Tranylcypromine
Major Depressive Disorder
Treatment of major depressive disorder without melancholia.
Efficacy in major depressive disorder with melancholia (endogenous features) not established.
MAO inhibitors appear particularly effective in treatment of major depressive disorder with atypical features, although other antidepressants (e.g., SSRIs) may initially be used because of their more favorable adverse effect profile.
Because of potential for serious adverse effects and necessity of dietary restrictions, MAO inhibitors (e.g., phenelzine, tranylcypromine) generally are not used as initial therapy for major depressive disorder, but are reserved for carefully selected patients who can be closely supervised and who have depression refractory to other antidepressants (e.g., SSRIs, SNRIs, TCAs) or in whom other therapies are contraindicated.
Tranylcypromine Dosage and Administration
General
-
Allow at least 1–2 weeks to elapse between discontinuance of therapy with another MAO inhibitor, dibenzazepine derivative (including carbamazepine and cyclobenzaprine), or TCA and initiation of tranylcypromine and vice versa.
-
Allow at least 2 weeks to elapse between discontinuance of tranylcypromine and initiation of bupropion.
-
Allow at least 2 weeks to elapse between discontinuance of an SSRI and initiation of tranylcypromine and vice versa. Also allow at least 5 weeks to elapse when switching from fluoxetine.
-
Allow at least 5 or 7 days to elapse between discontinuance of duloxetine or venlafaxine, respectively, and initiation of tranylcypromine and at least 2 weeks between discontinuance of tranylcypromine and initiation of duloxetine or venlafaxine.
-
Allow at least 10 days to elapse between discontinuance of tranylcypromine and initiation of buspirone.
-
Allow at least 2–3 weeks to elapse between discontinuance of tranylcypromine and meperidine administration.
-
Patients receiving tranylcypromine should be monitored for possible worsening of depression, suicidality, or unusual changes in behavior, especially at the beginning of therapy or during periods of dosage adjustment. (See Worsening of Depression and Suicidality Risk under Cautions.)
Administration
Oral Administration
Administer orally in divided doses. Administration earlier in the day (e.g., twice daily in the morning and afternoon) may reduce incidence of insomnia.
Dosage
Available as tranylcypromine sulfate; dosage expressed in terms of tranylcypromine.
Individualize dosage carefully according to individual requirements and tolerance.
Adults
Major Depressive Disorder
Oral
Usual dosage: 30 mg daily, usually given in 2 divided doses in the morning and afternoon. If no signs of therapeutic response appear after a reasonable period (up to 2–3 weeks), may increase dosage in increments of 10 mg daily at 1- to 3-week intervals until optimum therapeutic response or dosage of 60 mg daily is reached.
Dosages >30 mg daily may be associated with an increased frequency and severity of adverse effects. (See Orthostatic Hypotension under Cautions.) May reduce dosage to lower maintenance dosage once adequate response achieved.
Prescribing Limits
Adults
Major Depressive Disorder
Oral
Maximum 60 mg daily.
Cautions for Tranylcypromine
Contraindications
-
Concomitant administration of other MAO inhibitors (e.g., isocarboxazid, phenelzine, transdermal selegiline), dibenzazepine derivatives (e.g., amitriptyline, amoxapine, clomipramine, desipramine, doxepin, imipramine, maprotiline, nortriptyline, protriptyline, trimipramine, carbamazepine, cyclobenzaprine), centrally-acting sympathomimetic agents (e.g., amphetamines) or peripherally-acting sympathomimetic agents (prescription or OTC cold, hay fever, or weight-reducing preparations that contain vasoconstrictors), bupropion, buspirone, SNRIs (e.g., duloxetine, venlafaxine), SSRIs (e.g., citalopram, escitalopram, fluoxetine, fluvoxamine, paroxetine, sertraline), dexfenfluramine (no longer commercially available in US), meperidine and certain other CNS depressants (e.g., opiate analgesics, sedatives, anesthetics, alcohol), dextromethorphan, guanethidine, methyldopa, reserpine, antihypertensive agents, antiparkinsonian drugs (e.g., levodopa), diuretics, antihistamines, dopamine, tryptophan, consumption of excessive quantities of caffeine, and foods or beverages high in tyramine content. (See Interactions.)
-
Known or suspected cerebrovascular defects; cardiovascular disease or hypertension; history of headache.
-
Elective surgery requiring general anesthesia. Use of cocaine or local anesthesia containing sympathomimetic vasoconstrictors also not recommended. Consider possible combined hypotensive effects of tranylcypromine and spinal anesthesia. Discontinue tranylcypromine ≥10 days prior to elective surgery. (See Specific Drugs and Foods under Interactions.)
-
Pheochromocytoma.
-
History of liver disease or abnormal liver function tests.
Warnings/Precautions
Warnings
Shares the toxic potentials of other MAO inhibitors; observe the usual precautions and contraindications associated with therapy with these drugs. Should be used only by clinicians who are completely familiar with proper use, potential adverse effects, and associated precautions and contraindications of MAO inhibitors. Fully advise patients about risks, especially hypertensive crisis and suicidal thinking and behavior (suicidality), associated with MAO inhibitor therapy.
Worsening of Depression and Suicidality Risk
Possible worsening of depression and/or emergence of suicidal ideation and behavior (suicidality) or unusual changes in behavior in both adult and pediatric patients with major depressive disorder, whether or not they are taking antidepressants; may persist until clinically important remission occurs. However, suicide is a known risk of depression and certain other psychiatric disorders, and these disorders themselves are the strongest predictors of suicide.
Appropriately monitor and closely observe patients receiving tranylcypromine for any reason, particularly during initiation of therapy (i.e., the first few months) and during periods of dosage adjustments. (See Boxed Warning and also see Pediatric Use under Cautions.)
Anxiety, agitation, panic attacks, insomnia, irritability, hostility, aggressiveness, impulsivity, akathisia, hypomania, and/or mania may be precursors to emerging suicidality. Consider changing or discontinuing therapy in patients whose depression is persistently worse or in those with emerging suicidality or symptoms that might be precursors to worsening depression or suicidality, particularly if severe, abrupt in onset, or not part of patient’s presenting symptoms.
Prescribe in smallest quantity consistent with good patient management to reduce risk of overdosage.
Observe these precautions for patients with psychiatric (e.g., major depressive disorder, obsessive-compulsive disorder) or nonpsychiatric disorders.
Bipolar Disorder
May unmask bipolar disorder. (See Activation of Mania or Hypomania under Cautions.) Tranylcypromine is not approved for use in treating bipolar depression.
Screen for risk of bipolar disorder by obtaining detailed psychiatric history (e.g., family history of suicide, bipolar disorder, depression) prior to initiating therapy.
Hypertensive Crises
Hypertensive crises, sometimes fatal, are one of the most serious adverse effects associated with MAO inhibitors, including tranylcypromine. Although spontaneous cases reported, most cases occurred following ingestion of foods or beverages containing large amounts of tyramine (i.e., cheese reaction) or when MAO inhibitors were used concomitantly with certain prescription or OTC drugs. (See Specific Drugs and Foods under Interactions and see also Advice to Patients.)
Characterized by occipital headache (which may radiate frontally), palpitation, neck stiffness or soreness, nausea or vomiting, sweating (sometimes with fever or cold, clammy skin), mydriasis and/or visual disturbances (e.g., photophobia). Tachycardia or bradycardia with associated constricting chest pain and dilated pupils and intracranial hemorrhage, sometimes fatal, also reported.
Closely monitor BP in all patients to detect evidence of pressor response; however, full reliance should not be placed on BP determinations alone. Frequently observe patient’s clinical status, particularly for signs and symptoms of hypertension.
If a hypertensive crisis or prodromal signs of hypertensive crisis occur, discontinue MAO inhibitor therapy and immediately institute appropriate therapy to lower BP. Phentolamine considered hypotensive drug of choice for treating MAO inhibitor-induced hypertensive crisis. Manage fever by external cooling. Other symptomatic and supportive measures may be necessary in some patients; however, avoid administration of parenteral reserpine. (See Contraindications under Cautions and see Specific Drugs and Foods under Interactions.)
General Precautions
Activation of Mania or Hypomania
Possible activation of mania and hypomania, particularly in patients with bipolar disorder. (See Bipolar Disorder under Cautions.)
Orthostatic Hypotension
Possible hypotension. Postural hypotension symptoms most commonly observed in patients with preexisting hypertension. BP generally returns rapidly to pretreatment levels upon drug discontinuance.
At dosages >30 mg daily, postural hypotension is an important adverse effect and may cause syncope. In patients who show some hypotensive response during initiation of MAO inhibitor therapy, increase dosage more gradually. May relieve postural hypotension by having patient lie down until BP returns to normal.
Myelography
Avoid concurrent use of drugs that lower seizure threshold, including MAO inhibitors, and metrizamide (no longer commercially available in US). Discontinue tranylcypromine ≥48 hours prior to myelography; do not resume therapy for ≥24–48 hours post-procedure. (See Specific Drugs and Foods under Interactions.)
Cardiovascular Effects
MAO inhibitors may suppress anginal pain that would otherwise serve as a warning sign of myocardial ischemia; warn patients with angina pectoris or coronary artery disease against overexertion.
Endocrine and Metabolic Effects
MAO inhibitors may cause hypoglycemic episodes in diabetic patients receiving insulin or oral antidiabetic agents; use tranylcypromine with caution in diabetic patients receiving these drugs concurrently.
Use MAO inhibitors with caution in patients with hyperthyroidism, since these patients have an increased sensitivity to pressor amines.
Nervous System Effects
Possible aggravation of coexisting depressive symptoms, such as anxiety and agitation. (See Worsening of Depression and Suicidality Risk under Cautions.)
Overstimulation, including increased anxiety, agitation, and manic symptoms, may occur and usually indicates excessive therapeutic action; consider tranylcypromine dosage reduction or addition of antipsychotic (e.g., phenothiazine) therapy. (See Specific Drugs and Foods under Interactions.)
Seizures
MAO inhibitors have a variable effect on the seizure threshold; use with caution in patients with a seizure disorder.
Dependence and Withdrawal of Therapy
Drug dependence reported in patients receiving tranylcypromine dosages substantially in excess of usual therapeutic range; some of these patients had a history of previous substance abuse. Withdrawal symptoms reported include restlessness, anxiety, depression, confusion, hallucinations, headache, weakness, and diarrhea.
Specific Populations
Pregnancy
Category C.
Lactation
Distributes into milk. Caution if used in nursing women.
Pediatric Use
Safety and efficacy in pediatric patients not established.
FDA warns that a greater risk of suicidal thinking or behavior (suicidality) occurred during first few months of antidepressant treatment (4%) compared with placebo (2%) in children and adolescents with major depressive disorder, obsessive-compulsive disorder (OCD), or other psychiatric disorders based on pooled analyses of 24 short-term, placebo-controlled trials of 9 antidepressant drugs (SSRIs and others). However, a more recent meta-analysis of 27 placebo-controlled trials of 9 antidepressants (SSRIs and others) in patients <19 years of age with major depressive disorder, OCD, or non-OCD anxiety disorders suggests that the benefits of antidepressant therapy in treating these conditions may outweigh the risks of suicidal behavior or suicidal ideation. No suicides occurred in these pediatric trials.
Carefully consider these findings when assessing potential benefits and risks of tranylcypromine in a child or adolescent for any clinical use. (See Worsening of Depression and Suicidality Risk under Cautions.)
Geriatric Use
Clinical experience with MAO inhibitors has not identified any differences in responses between geriatric and younger adults.
In pooled data analyses, a reduced risk of suicidality was observed in adults ≥65 years of age with antidepressant therapy compared with placebo. (See Boxed Warning and also see Worsening of Depression and Suicidality Risk under Cautions.)
Possible increased morbidity during or following episodes of hypertension or malignant hyperthermia; geriatric patients have less compensatory reserve to cope with any serious adverse reaction.
Use with caution.
Hepatic Impairment
Contraindicated in patients with history of hepatic disease or abnormal liver function test results.
Renal Impairment
Possible accumulation of tranylcypromine in plasma; use with caution.
Common Adverse Effects
Adverse nervous system effects (e.g., insomnia, dizziness, headache), GI effects (e.g., dry mouth, anorexia, nausea, diarrhea, abdominal pain, constipation), cardiovascular effects (e.g., orthostatic hypotension, hypertension, tachycardia, peripheral edema, palpitation), GU effects (e.g., impotence, delayed ejaculation, urinary retention), blurred vision, chills, weight gain.
Drug Interactions
Drugs Associated with Serotonin Syndrome
Potential pharmacologic interaction (serotonin syndrome) with serotonergic agents. Caution generally advised. (See Specific Drugs and Foods under Interactions.)
Specific Drugs and Foods
|
Drug or Food |
Interaction |
Comments |
|---|---|---|
|
Alcohol |
May potentiate action of alcohol Possible hypertensive crisis with tyramine-containing alcoholic beverages (e.g., Chianti wine, beer, liqueurs) |
Concomitant use contraindicated |
|
Anesthetics |
General anesthetics: Possible exaggeration of hypotensive and CNS depressant effects Local anesthesia with cocaine or local anesthetics that contain sympathomimetic vasoconstrictors: Possible hypertension Spinal anesthesia: Possible potentiation of the hypotensive effect of local anesthetics |
For elective surgery, discontinue tranylcypromine for ≥10 days prior to elective surgery with general anesthetics; for emergency surgery, carefully adjust dosage of general anesthetics Local anesthesia with cocaine or local anesthetics that contain sympathomimetic vasoconstrictors: Avoid concomitant use Spinal anesthesia: Use with caution |
|
Antidepressants, SNRIs (e.g., duloxetine, venlafaxine) |
Potentially life-threatening serotonin syndrome |
Concomitant use contraindicated Allow at least 5 or 7 days to elapse between discontinuance of duloxetine or venlafaxine, respectively, and initiation of tranylcypromine and at least 2 weeks between discontinuance of tranylcypromine and initiation of duloxetine or venlafaxine |
|
Antidepressants, SSRIs (e.g., citalopram, escitalopram, fluoxetine, fluvoxamine, paroxetine, sertraline) |
Potentially life-threatening serotonin syndrome or neuroleptic malignant syndrome (NMS) |
Concomitant use contraindicated Allow at least 2 weeks to elapse between discontinuance of tranylcypromine and initiation of an SSRI, and vice versa Allow at least 5 weeks to elapse between discontinuance of fluoxetine and initiation of tranylcypromine |
|
Antidepressants, tricyclic (TCAs) (e.g., amitriptyline, desipramine, imipramine, nortriptyline, protriptyline) |
Potentially life-threatening serotonin syndrome |
Concomitant use contraindicated Allow at least 1–2 weeks to elapse when switching to or from these drugs |
|
Antidiabetic agents, oral |
Possible hypoglycemic episodes |
Use with caution |
|
Antihypertensive agents |
Potential marked hypotensive effect |
Generally should avoid concomitant use |
|
Bupropion |
Possible enhanced acute toxicity of bupropion |
Concurrent administration is contraindicated; at least 2 weeks should elapse between discontinuance of tranylcypromine and initiation of bupropion |
|
Buspirone |
Elevated BP reported with concomitant use; possible serotonin syndrome |
Concomitant use contraindicated Allow at least 10 days to elapse between discontinuance of tranylcypromine and initiation of buspirone |
|
Caffeine |
May precipitate hypertensive crisis if taken in excessive quantities |
Concomitant use of excessive quantities of caffeine contraindicated |
|
Carbamazepine |
Hypertensive crises or severe seizures may occur; possible serotonin syndrome |
Concomitant use contraindicated Allow at least 1–2 weeks to elapse between discontinuance of tranylcypromine and initiation of carbamazepine and vice versa |
|
CNS depressants (e.g., opiate analgesics) |
May potentiate the action of CNS depressants |
Concomitant use contraindicated |
|
Cyclobenzaprine |
Possible hypertensive crises or severe seizures |
Concomitant use contraindicated Allow at least 1–2 weeks to elapse between discontinuance of tranylcypromine and initiation of cyclobenzaprine and vice versa |
|
Dextromethorphan |
Brief episodes of psychosis or bizarre behavior reported; possible serotonin syndrome |
Concomitant use contraindicated |
|
Disulfiram |
Delirium reported in humans; severe toxicity, including seizures and death, reported during concurrent administration in animals in 1 study but no adverse interactions reported in other animal studies |
Use with caution |
|
Diuretics |
Potential marked hypotensive effect |
Generally should avoid concomitant use |
|
Foods and beverages, tyramine-containing (e.g., cheese, sour cream, Chianti wine, sherry, beer, liqueurs, pickled herring, anchovies, caviar, liver, canned figs, dried fruits, bananas, raspberries, overripe fruit, chocolate, soy sauce, sauerkraut, fava beans, yeast extracts, yogurt, dry sausage, meat extracts or meat prepared with tenderizers) |
Serious, sometimes fatal hypertensive reactions (e.g., palpitation, headache, nausea, vomiting, photophobia, diaphoresis) reported |
Avoid foods and beverages with high tyramine content (e.g., cheese) Consult specialized references on food constituents or dietician for specific information on tyramine content of foods and beverages |
|
Guanethidine |
Possible severe pressor response |
Concomitant use contraindicated |
|
Insulin |
Possible hypoglycemic episodes |
Use with caution |
|
Levodopa-carbidopa |
Potential for hypertension, headache, hyperexcitability, and related symptoms |
Concomitant use contraindicated Discontinue tranylcypromine ≥2 weeks prior to initiation of levodopa |
|
MAO inhibitors (e.g., isocarboxazid, phenelzine, transdermal selegiline) |
Hypertensive crises or severe seizures may occur with concomitant administration |
Concomitant use contraindicated Allow at least 1 week to elapse between discontinuance of another MAO inhibitor and initiation/re-initiation of tranylcypromine, or vice versa |
|
Meperidine |
Severe, generally immediate reactions, including excitation, sweating, rigidity, respiratory depression, seizures, hypertension or hypotension, coma, and death, suggestive of serotonin syndrome reported |
Concomitant use contraindicated Allow at least 2–3 weeks to elapse between discontinuance of tranylcypromine and administration of meperidine |
|
Methyldopa |
Potential for hypertension, headache, hyperexcitability, and related symptoms |
Concomitant use contraindicated |
|
Metrizamide (no longer commercially available in US) |
Possible increased risk of seizures |
Discontinue tranylcypromine ≥48 hours prior to myelography; do not resume therapy for ≥24–48 hours post-procedure |
|
Modafinil |
Acute dyskinesia, confusion, and hyperthermia reported during concurrent administration; possible increased dopaminergic and serotonergic activity |
|
|
Phenothiazines |
Possible additive hypotensive effects |
|
|
Reserpine |
Possible severe pressor response |
Concomitant use contraindicated (see Hypertensive Crises under Cautions) |
|
Sympathomimetic agents (e.g., amphetamine, dopamine, OTC cold, hay fever, or weight-reducing preparations) |
Possible hypertensive crisis and serotonin syndrome |
Concomitant use contraindicated |
|
Tryptophan |
Possible behavioral and neurological symptoms suggestive of serotonin syndrome |
Concomitant use contraindicated |
Tranylcypromine Pharmacokinetics
Absorption
Bioavailability
Rapidly absorbed following single-dose (20 mg), oral administration, with peak plasma tranylcypromine concentrations of approximately 110 ng/mL (range: 65–190 ng/mL) achieved within approximately 1.5 hours (range: 0.7–3.5 hours). GI absorption demonstrates interindividual variation and may be biphasic in some individuals.
Onset
Pharmacologic effects of MAO inhibitors are cumulative; onset of pharmacologic action of tranylcypromine is more rapid than that of hydrazine-derivative MAO inhibitors (e.g., phenelzine). Antidepressant effect usually evident within 2 days–3 weeks.
Duration
Inhibition of MAO may persist up to 10 days following drug discontinuance.
Distribution
Extent
Crosses placenta in rats. Distributes into human milk.
Elimination
Metabolism
Rapidly and extensively metabolized following oral administration.
Elimination Route
Excretion is rapid, occurring within 24 hours after drug discontinuance; however, urinary tryptamine concentrations, which are used to measure MAO activity, return to normal within 72–120 hours.
Half-life
Elimination half-life averages 2.5 hours (range: 1.5–3.2 hours).
Stability
Storage
Oral
Tablets
Well closed, light-resistant containers at 20–25°C (may be exposed to 15–30°C).
Actions
-
Principal pharmacologic effects of tranylcypromine are similar to those of other nonselective MAO inhibitors (e.g., phenelzine).
-
Tranylcypromine binds reversibly to the MAO enzyme while phenelzine binds irreversibly to the enzyme.
-
Precise mechanism of antidepressant action is unknown but may involve increases in free serotonin and norepinephrine and/or alterations in other amine concentrations within the CNS.
Advice to Patients
-
Risk of suicidality; importance of patients, family, and caregivers being alert to and immediately reporting emergence of suicidality, worsening depression, or unusual changes in behavior, especially during the first few months of therapy or during periods of dosage adjustment. FDA recommends providing written patient information (medication guide) explaining risks of suicidality each time the drug is dispensed.
-
Risk of serious adverse effects (e.g., hypertensive reactions). Importance of promptly informing clinicians if headache or other unusual symptoms (e.g., palpitation and/or tachycardia, constriction in throat or chest, sweating, dizziness, neck stiffness, nausea or vomiting) occur.
-
Importance of informing patients to avoid foods and beverages with a high tyramine content.
-
Importance of informing patients to avoid excessive use of caffeine in any form.
-
Importance of informing patients to avoid alcoholic beverages.
-
Risk of hypotension, faintness, and drowsiness. Importance of considering possible impaired ability to perform hazardous activities (e.g., operating machinery, driving a motor vehicle).
-
Importance of patients informing their clinicians and dentist that they are taking tranylcypromine.
-
Importance of women informing their clinician if they are or plan to become pregnant or plan to breast-feed.
-
Importance of informing clinicians of existing or contemplated concomitant therapy, including prescription and OTC drugs and herbal or nutritional supplements, as well as any concomitant illnesses.
-
Importance of informing patients of other important precautionary information. (See Cautions.)
Preparations
Excipients in commercially available drug preparations may have clinically important effects in some individuals; consult specific product labeling for details.
Please refer to the ASHP Drug Shortages Resource Center for information on shortages of one or more of these preparations.
|
Routes |
Dosage Forms |
Strengths |
Brand Names |
Manufacturer |
|---|---|---|---|---|
|
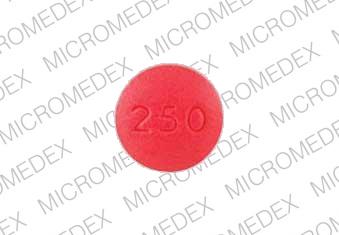
Oral |
Tablets, film-coated |
10 mg (of tranylcypromine) |
Parnate |
GlaxoSmithKline |
|
Tranylcypromine Sulfate |
Par |
AHFS DI Essentials™. © Copyright 2024, Selected Revisions July 1, 2008. American Society of Health-System Pharmacists, Inc., 4500 East-West Highway, Suite 900, Bethesda, Maryland 20814.
Reload page with references included
Frequently asked questions
More about tranylcypromine
- Check interactions
- Compare alternatives
- Pricing & coupons
- Reviews (123)
- Drug images
- Side effects
- Dosage information
- During pregnancy
- Drug class: monoamine oxidase inhibitors
- Breastfeeding
- En español